If you’re pregnant or have recently given birth, you’ve probably seen those mysterious numbers on the hospital monitor during labor. One of the most common questions expectant mothers ask is: what does the toco number mean? Understanding these numbers can help reduce anxiety during labor and help you better communicate with your healthcare team. Let’s explore everything you need to know about toco numbers and why they matter during childbirth.
Understanding the Toco Monitor
Before diving into what does the toco number mean, it’s important to understand what the toco monitor actually measures. “Toco” is short for tocodynamometer, a device that measures the strength and frequency of uterine contractions during labor.
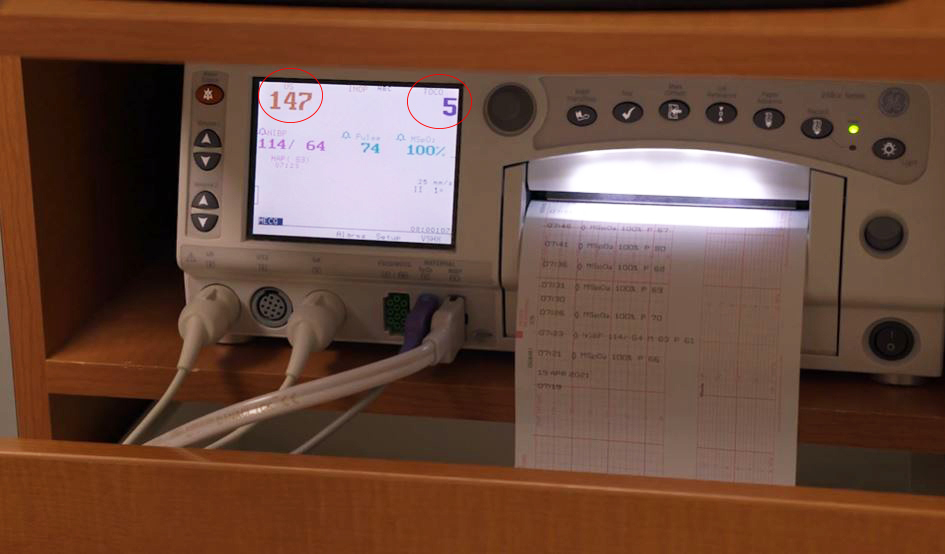
The toco monitor is part of the external fetal monitoring system used in hospitals and birthing centers. It’s a flat, round sensor placed on your belly that detects the tightening and relaxing of your uterus during contractions. The device converts these physical changes into numbers that appear on a screen, helping your medical team track your labor progress.
What Toco Numbers Actually Measure
So, what does the toco number mean exactly? Toco numbers measure the intensity of uterine contractions in arbitrary units. Unlike blood pressure or temperature, these numbers don’t represent a specific medical measurement like millimeters of mercury or degrees Fahrenheit.
Instead, toco numbers show relative contraction strength. The baseline reading when your uterus is relaxed might be anywhere from 5 to 20 units. During a contraction, the numbers rise, sometimes reaching 50, 80, or even higher than 100 units depending on the strength of the contraction.
The Baseline Reading
Your baseline toco number is what the monitor shows when you’re not having a contraction. This typically ranges between 5 and 20 units, though it can vary based on how the monitor is positioned, your body type, and how relaxed your uterine muscles are between contractions.
Peak Contraction Numbers
During a contraction, toco numbers rise significantly. Early labor contractions might increase the reading to 40-60 units, while active labor contractions often reach 60-80 units or higher. Transition phase contractions—the strongest and most intense—can push toco numbers above 100 units.
Why Toco Numbers Vary So Much
Understanding what does the toco number mean requires knowing why these numbers can be so different from person to person and even from contraction to contraction for the same person.
Individual Body Differences
Every woman’s body is unique. Factors like belly size, the amount of amniotic fluid, baby’s position, and abdominal muscle tone all affect toco readings. A thinner person might show higher numbers for the same contraction intensity compared to someone with more abdominal tissue.
Monitor Placement
Where the toco sensor is placed on your belly significantly impacts the readings. If the sensor is positioned directly over where contractions are strongest, numbers will be higher. If it shifts or isn’t optimally placed, numbers might appear lower even though contraction intensity hasn’t changed.
Movement and Position Changes
When you move during labor—which is actually encouraged—the toco monitor can shift, causing number fluctuations that don’t reflect actual changes in contraction strength. This is completely normal and why nurses frequently adjust the monitor placement.
Reading Toco Numbers During Different Labor Stages
What does the toco number mean changes depending on which stage of labor you’re experiencing. Let’s break down typical toco readings for each phase.
Early Labor
During early labor, toco numbers might rise to 40-60 units during contractions. These contractions are usually irregular and may feel like strong menstrual cramps. The baseline between contractions remains around 5-20 units.
At this stage, contractions are working to efface (thin) and begin dilating your cervix. The relatively lower toco numbers reflect the gradual nature of early labor.
Active Labor
Active labor brings stronger, more regular contractions. Toco numbers during this phase typically reach 60-80 units or higher. The baseline may remain similar, but the peaks are noticeably higher and occur more frequently—usually every 3-5 minutes.
These stronger contractions are doing the important work of dilating your cervix from about 6 centimeters to 10 centimeters, preparing for delivery.
Transition Phase
Transition is the most intense part of labor, and toco numbers reflect this intensity. Readings during transition contractions often exceed 80-100 units and can sometimes reach even higher. These contractions come very close together, sometimes with only a minute or two of rest between them.
While transition is the shortest phase of labor, it’s also the most challenging, and the high toco numbers validate what you’re feeling.
Pushing Stage
During pushing, toco numbers may actually appear lower on the monitor, but this doesn’t mean contractions are weaker. The reading might seem inconsistent because you’re actively bearing down, which can affect how the external monitor reads your contractions.
For more health information explained in simple terms, visit blog arcyart for comprehensive guides on pregnancy, childbirth, and family wellness.
What Toco Numbers Don’t Tell You
While understanding what does the toco number mean is helpful, it’s equally important to know the limitations of these readings.
Not a Measure of Pain
Toco numbers don’t measure your pain level. One woman might have contractions registering at 70 units and feel manageable discomfort, while another might experience contractions at the same level as extremely painful. Pain perception is individual and influenced by many factors beyond contraction strength.
Not the Only Important Indicator
Healthcare providers consider toco numbers alongside many other factors: cervical dilation and effacement, baby’s heart rate, your vital signs, and how you’re coping with labor. Toco numbers are just one piece of the puzzle.
Internal vs. External Monitoring
External toco monitoring provides useful information, but it’s less precise than internal monitoring. If your healthcare team needs more accurate contraction measurements, they might use an intrauterine pressure catheter (IUPC), which measures actual pressure inside your uterus in millimeters of mercury.
How Healthcare Providers Use Toco Numbers
Medical professionals don’t rely solely on the question what does the toco number mean when making decisions about your care. They use toco readings as part of a comprehensive assessment.
Tracking Labor Progression
Nurses and doctors watch toco numbers to understand your contraction pattern—how often contractions occur, how long they last, and whether they’re becoming more regular and intense over time. This helps them gauge whether labor is progressing normally.
Timing Interventions
Healthcare providers may use toco readings to time certain interventions. For example, if contractions are weak or irregular, they might discuss options like walking, position changes, or medication to strengthen labor.
Monitoring Baby’s Response
Toco numbers are always viewed alongside the baby’s heart rate monitor. Healthcare teams look at how the baby’s heart rate responds to contractions, ensuring the baby tolerates labor well.
Common Toco Number Ranges
While every labor is unique, here are general ranges that help answer what does the toco number mean for most women:
| Labor Stage | Typical Toco Range | Contraction Frequency |
|---|---|---|
| Resting Baseline | 5-20 units | No contraction |
| Early Labor | 40-60 units | Irregular, 15-20 min apart |
| Active Labor | 60-80 units | Every 3-5 minutes |
| Transition | 80-100+ units | Every 2-3 minutes |
| Pushing Stage | Variable | Every 2-3 minutes |
Remember, these are general guidelines. Your numbers might be higher or lower and still be completely normal for your labor.
When Toco Numbers Might Concern Your Healthcare Team
Healthcare providers watch for certain patterns in toco readings that might indicate complications or the need for intervention.
Tachysystole
This term describes too-frequent contractions—more than five in 10 minutes. When contractions come too close together, the baby might not get enough recovery time between them. Your healthcare team watches toco patterns to identify and address this issue.
Weak Contractions
If toco numbers consistently stay low (below 40-50 units) during active labor and your cervix isn’t dilating as expected, your provider might discuss ways to strengthen contractions, such as breaking your water or using medication.
Irregular Patterns
Contractions that start and stop without establishing a regular pattern might indicate labor hasn’t fully established. Your healthcare team uses toco readings combined with cervical exams to determine the best course of action.
What You Should Focus On Instead
While it’s natural to watch the monitor and wonder what does the toco number mean, there are more important things to focus on during labor.
Your Body’s Signals
Pay attention to what your body is telling you. How intense do contractions feel? Are you able to breathe through them? Do you need pain management? Your subjective experience matters more than any number on a screen.
Relaxation and Coping
Focus your energy on relaxation techniques, breathing exercises, and coping strategies rather than watching numbers climb. Trust that your healthcare team is monitoring everything and will let you know if something needs attention.
Communication with Your Team
Instead of interpreting toco numbers yourself, communicate openly with your nurses and doctors about what you’re feeling. They can explain what the numbers mean in the context of your specific labor.
Toco Monitoring and Pain Management Decisions
Understanding what does the toco number mean can sometimes help with decisions about pain management during labor.
Timing Epidural Placement
Some women find it helpful to see their contraction pattern on the monitor when deciding about pain relief. Knowing that contractions are becoming stronger and more frequent might influence your decision about when to request an epidural.
Evaluating Pain Relief Effectiveness
After receiving pain medication or an epidural, you might still see high toco numbers even though you feel less pain. This shows the medication is working—contractions continue doing their job while you experience less discomfort.
Toco Monitoring During Induction
If your labor is being induced with medication like Pitocin, toco monitoring becomes especially important for your healthcare team.
Adjusting Medication Dosage
Nurses closely watch toco numbers during induction to adjust Pitocin dosage. They want contractions strong enough to progress labor but not so frequent that they stress the baby.
Preventing Hyperstimulation
Toco monitoring helps identify if induced contractions are too strong or too frequent. If numbers indicate hyperstimulation, the medical team can quickly decrease or stop medication to protect both you and your baby.
Technology and Toco Monitoring
Modern labor and delivery units use advanced monitoring technology that makes interpreting what does the toco number mean easier for healthcare providers.
Digital Displays
Most hospitals now use digital monitors that display both toco numbers and the baby’s heart rate simultaneously. These screens often show the readings as graphs over time, making patterns easier to identify.
Remote Monitoring
Many hospitals have systems that allow nurses and doctors to view your monitor readings from the nurses’ station or even remotely. This means someone is always keeping an eye on your labor progress, even when they’re not physically in your room.
Wireless Options
Some facilities offer wireless monitoring systems that allow you to move more freely during labor while still being monitored. These systems use the same technology to measure contractions but give you more mobility.
Conclusion
So, what does the toco number mean? Toco numbers measure the relative strength of your uterine contractions during labor using arbitrary units that typically range from a resting baseline of 5-20 units to peaks of 40-100+ units during contractions. While these numbers provide useful information for your healthcare team, they’re just one tool among many for monitoring your labor. The numbers can vary based on body type, monitor placement, and individual differences, and they don’t measure pain levels. Instead of focusing too much on the numbers, trust your healthcare providers to interpret them while you concentrate on working with your body during this amazing journey of bringing your baby into the world. Remember, every labor is unique, and your experience is what truly matters, not any number on a screen.
| Toco Number Quick Reference | Information |
|---|---|
| What Toco Stands For | Tocodynamometer |
| What It Measures | Uterine contraction intensity |
| Units | Arbitrary units (not standardized) |
| Resting Baseline | 5-20 units |
| Early Labor Peak | 40-60 units |
| Active Labor Peak | 60-80 units |
| Transition Peak | 80-100+ units |
| Does It Measure Pain? | No—only contraction strength |